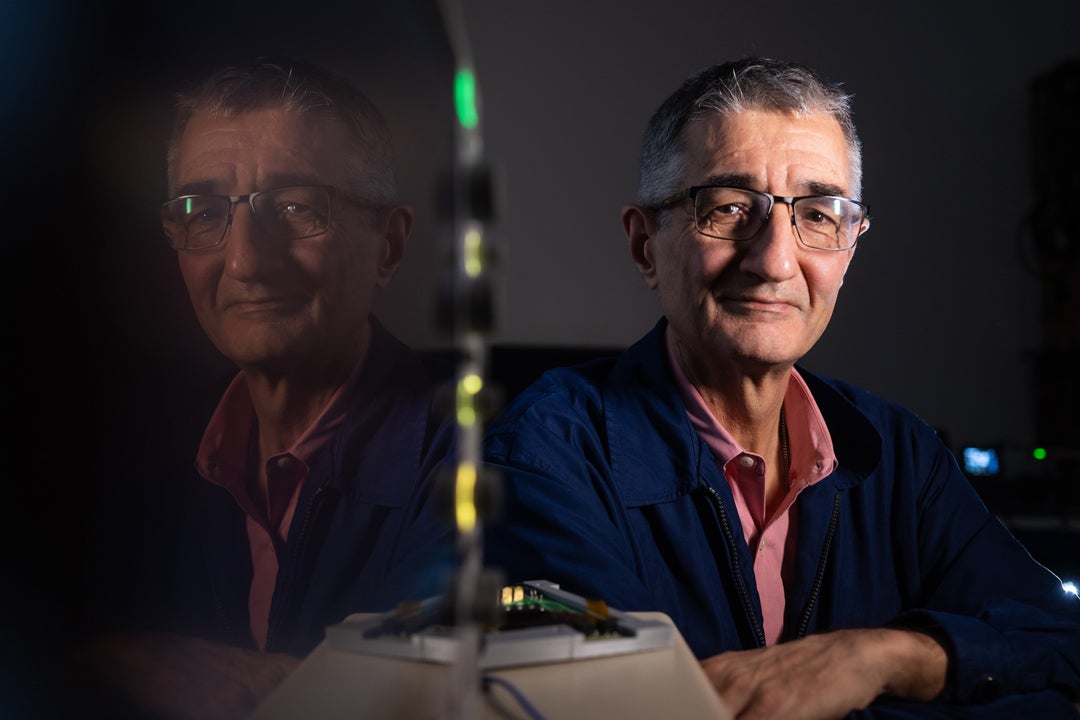
Physicists have studied subatomic particles for over a hundred years, trying to unlock the universe's deepest secrets. Pablo Yepes’ fascination with these particles began as a fundamental curiosity about the subatomic nature of matter and radiation that make up the universe we observe. These days, his work focuses on the use of subatomic particles, specifically protons, to precisely target and destroy cancer cells in the human body.
“My background is in particle physics,” said Yepes, a research professor of physics and astronomy. As a member of the STAR Collaboration at the Relativistic Heavy Ion Collider at Brookhaven National Laboratory, Yepes developed algorithms to monitor and analyze the results of heavy ions colliding. These methods are still in use at large accelerators, including the European Center for Nuclear Research (CERN).
“Technically, it's very similar,” Yepes explained. “In one case, you are shooting particles into a detector. In the other, you shoot particles into a person.” Using his expertise from Brookhaven and CERN, Yepes has developed methods to accurately calculate the amount and energy of protons necessary to irradiate a tumor, while sparing the surrounding healthy tissue. “Algorithms that are now standard for medical physics were actually developed by people at CERN,” he shared.
Most commonly, radiation therapies use X-rays, gamma rays or electrons to target a tumor. As the name suggests, proton therapy (PT) uses protons to treat cancer and some non-cancerous tumors. Similar to a beam of light from a laser pointer, a beam of protons is used to target a tumor. Such high-energy beams are generated with particle accelerators called cyclotrons.
“Why protons instead of the others?” Yepes asked. “The main reason is that protons stop, while most of the photons and electrons go through.” The differentiated penetration of a proton beam minimizes secondary effects when treating patients with PT, he said.

“For example, if you’re treating cancer on the spine, you could illuminate with X-rays from the back, but the rays will go through and damage the patient’s internal organs,” he explained. “With protons, it is possible to tune the beam so they stop at the tumor, minimizing exposure to the tissue before, and preventing them from reaching tissue behind, the tumor.”
Still, to optimally use PT, further understanding of the interaction between protons and different kinds of tissues is needed. “Protons are more sensitive to the medium,” Yepes said. “Information from other kinds of radiation, like X-rays in a CAT scan, can be used to calculate a proton dose. However, that information limits the accuracy of the calculations for protons.” Moreover, the biological effects of a beam of X-rays or electrons are not the same as those of a beam of protons with the same energy. Yepes collaborates with physicians and medical physicists at the University of Texas MD Anderson Cancer Center by using his methods to improve patient treatment.
“Doctors work with doses,” he explained. “So you need to calculate a dose to treat a patient. This calculation used to be done with analytical methods that were fast, but not always accurate, especially in regions of the body with many different types of tissue, like the chest or the head.” The Fast Dose Calculator, developed by Yepes, drastically reduces calculation times without significantly compromising the accuracy of the dose.
Another of Yepes’ methods predicts the amount of energy delivered by a proton beam as it travels through tissue, a measure dubbed “linear energy transfer,” or LET. By accurately predicting how the proton beam is absorbed by the different tissues it penetrates, collateral damage to healthy tissue can be further diminished.
“Ongoing medical trials are testing whether patients treated with a plan that optimizes LET show significantly less damage to healthy tissue after treatment,” Yepes said.
— Andrés B. Sánchez-Alvarado